Navigating infection control requires readily available resources. Numerous guidelines, checklists, and forms – like those from WHO and national sources – aid understanding and implementation.
What is Infection Control and Why is it Important?
Infection control encompasses strategies designed to prevent the spread of infections within healthcare settings and the community. It’s a critical component of patient safety, protecting both individuals receiving care and healthcare personnel.
Effective infection control minimizes Healthcare-Associated Infections (HAIs), reducing morbidity, mortality, and healthcare costs. National guidelines and resources, including checklists for PIIK and standardized HAI definitions, are vital.
Understanding various disinfection technologies, alongside consistent hand hygiene monitoring (using WHO forms), strengthens these efforts. Proactive infection control isn’t merely a procedural requirement; it’s a fundamental ethical obligation ensuring quality care and public health protection.
The Role of Standard Precautions
Standard Precautions represent the foundational level of infection control, applied to all patients, regardless of their presumed infection status. This approach minimizes the risk of transmission from both recognized and unrecognized sources of infection.
Key elements include hand hygiene, use of personal protective equipment (PPE) – gloves, gowns, masks – respiratory hygiene/cough etiquette, safe injection practices, and proper handling of potentially contaminated surfaces and items.
Implementing Standard Precautions consistently, across all levels of care (primary, secondary, tertiary), requires a well-defined organizational chart and adherence to minimum IPC criteria. These measures are essential for creating a safer healthcare environment, as highlighted in national guidelines.

Common Infection Control Questions
Frequently asked questions about infection prevention are crucial for clarity. Addressing these concerns ensures consistent practices and a safer environment for everyone involved.
What are the Key Elements of Hand Hygiene?

Effective hand hygiene is a cornerstone of infection control, encompassing several vital elements. These include using either soap and water or an alcohol-based hand rub. The process requires covering all surfaces of the hands – palms, backs, between fingers, and under nails – with the chosen agent.
Duration is also critical; handwashing with soap and water should last at least 20-30 seconds, while alcohol-based rubs need approximately 20-30 seconds to dry.
Proper technique is paramount, ensuring thorough cleaning without recontamination. Resources like WHO guidelines and self-assessment forms (Annex 6) provide detailed instructions and monitoring tools to optimize hand hygiene practices within healthcare settings and beyond.
How Often Should Hands Be Washed?
The frequency of handwashing is dictated by risk assessment and specific circumstances. Hands should always be washed before and after direct patient contact, after removing personal protective equipment (PPE), and after contact with potentially contaminated surfaces or fluids.
Crucially, wash hands before performing aseptic tasks, like inserting an IV, and after body fluid exposure risk.
Monitoring forms (WHO ⸺ Annex 8) can help track adherence to these practices. National guidelines (Dushanbe 2023) emphasize consistent hand hygiene as a fundamental infection prevention strategy, adapting frequency based on the level of care – primary, secondary, or tertiary – and potential exposure risks.
What are the Different Types of Hand Hygiene Techniques?
Effective hand hygiene encompasses several techniques, primarily handwashing with soap and water, and the use of alcohol-based hand rubs (ABHR). Handwashing requires at least 20-30 seconds, covering all surfaces.
ABHRs are efficient when hands are not visibly soiled, offering rapid germ reduction. Proper technique involves applying to all surfaces and rubbing until dry.
Self-assessment forms (Annex 6) can evaluate technique proficiency. National guidelines (Dushanbe 2023) and WHO resources detail these methods, emphasizing that consistent, correct application is paramount. Choosing the appropriate method depends on the situation and available resources, always prioritizing thoroughness.

Personal Protective Equipment (PPE)
PPE is crucial for minimizing exposure. Proper selection, donning, doffing, and consistent use are vital components of infection prevention protocols, as outlined in guidelines.
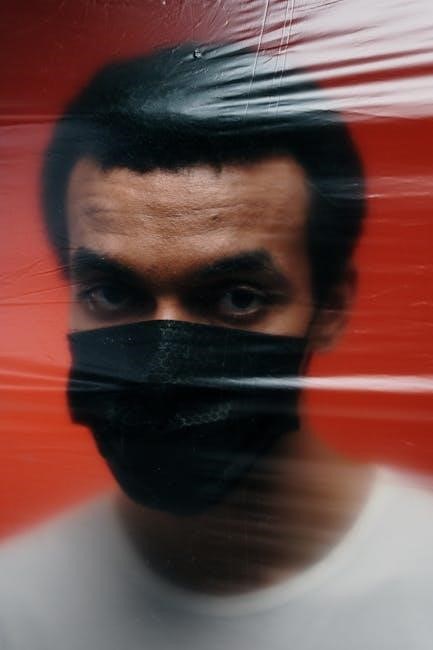
When is PPE Required?
Personal Protective Equipment (PPE) usage is dictated by risk assessment. It’s essential when anticipating contact with potentially infectious materials – blood, body fluids, secretions, excretions, contaminated items, or surfaces. Specific scenarios demanding PPE include procedures involving splashes or sprays, handling contaminated equipment, and during outbreaks of airborne diseases;
National guidelines and facility protocols clearly define when gloves, gowns, masks, eye protection (goggles or face shields), and respirators are necessary. Compliance hinges on understanding transmission-based precautions (contact, droplet, airborne) and adhering to established protocols. Regular training and readily accessible PPE are also paramount for consistent and correct application, safeguarding both healthcare workers and patients.
What are the Different Types of PPE and Their Proper Use?
Various PPE types offer specific protection. Gloves (latex, nitrile, vinyl) prevent contact with contaminants; gowns (disposable or reusable) protect skin and clothing. Masks shield the nose and mouth from droplets, while respirators (N95) filter airborne particles.
Eye protection – goggles or face shields – guards against splashes. Proper use involves correct donning and doffing procedures to avoid self-contamination. Gloves should fit snugly, gowns fully cover torso, and masks create a tight seal. PPE must be discarded appropriately after each use, or reusable items decontaminated according to facility protocols. Training on selection, fit-testing (for respirators), and proper use is crucial.
How to Don and Doff PPE Correctly
Correct PPE removal minimizes contamination risk. Donning (putting on) follows a specific sequence: gown, mask/respirator, goggles/face shield, then gloves. Doffing (taking off) is more complex and critical – gloves first, followed by gown, goggles/face shield, and finally, the mask/respirator, handling each item carefully to avoid touching contaminated surfaces.
Hand hygiene is essential before donning and after doffing. Designated areas for donning/doffing are recommended. Proper disposal of single-use items is vital. Training and observation are key to ensuring staff competency. Incorrect doffing is a frequent source of self-contamination, highlighting the need for meticulous adherence to protocols.

Environmental Infection Control
Maintaining clean surfaces is crucial. Disinfection protocols, utilizing appropriate agents for various areas, alongside sterilization practices, prevent healthcare-associated infections effectively.
Disinfection vs. Sterilization: What’s the Difference?
Understanding the distinction between disinfection and sterilization is fundamental to effective infection control. Disinfection reduces the number of microorganisms on a surface to a safe level, but doesn’t necessarily eliminate all of them. Various disinfection technologies exist, each with unique features, as detailed in national guidelines and annexes.
Sterilization, however, is a much more rigorous process. It completely eliminates all forms of microbial life, including bacterial spores. This is typically achieved through methods like autoclaving or using specific chemical sterilants. The choice between disinfection and sterilization depends on the item and its intended use. Critical items, like surgical instruments, require sterilization, while non-critical items may only need disinfection.
Proper application of each process is vital, referencing established protocols for healthcare settings to minimize risks.
Appropriate Disinfectants for Different Surfaces
Selecting the right disinfectant is crucial for effective infection control, varying based on the surface material and the microorganisms targeted. National guidelines outline appropriate disinfectants for healthcare settings, emphasizing compatibility with surfaces to avoid damage.
For non-porous surfaces, such as metal or plastic, commonly used disinfectants include quaternary ammonium compounds and alcohol-based solutions. Porous surfaces, like fabrics or wood, may require stronger disinfectants like bleach solutions, though careful consideration of material compatibility is essential.

Always follow manufacturer’s instructions regarding dilution, contact time, and safety precautions. Annexes within infection control documents often detail various disinfection technologies and their specific applications, ensuring optimal efficacy and minimizing potential harm.
Cleaning and Disinfection Protocols for Healthcare Settings
Robust cleaning and disinfection protocols are foundational to preventing Healthcare-Associated Infections (HAIs). These protocols must adhere to national guidelines and be tailored to the specific healthcare setting – primary, secondary, or tertiary care – with minimum criteria established for each level.
Protocols typically involve a two-step process: cleaning to remove visible soil, followed by disinfection to eliminate microorganisms. Regularly scheduled cleaning of high-touch surfaces, like doorknobs and bedside tables, is paramount.
Detailed checklists (Annex 4 in some national guidelines) ensure consistent application of these protocols. Proper documentation and monitoring (using WHO Hand Hygiene Monitoring Forms as an example) are vital for assessing effectiveness and identifying areas for improvement.
Healthcare-Associated Infections (HAIs)
HAIs demand vigilant prevention strategies. Standard definitions and reporting forms (Annex 7) are crucial for surveillance and tracking infection rates effectively.
What are HAIs and How are They Prevented?
Healthcare-Associated Infections (HAIs), formerly known as nosocomial infections, are infections patients acquire during healthcare delivery. Prevention hinges on a multi-faceted approach, beginning with strict adherence to standard precautions – hand hygiene being paramount.
Effective strategies include meticulous environmental cleaning and disinfection, utilizing appropriate disinfectants for various surfaces. Proper management of sharps injuries and spill protocols are also vital. Surveillance systems, utilizing standardized definitions and reporting forms (as outlined in Annex 7), allow for tracking and analysis of HAI incidence.
Furthermore, robust infection control programs, with clearly defined organizational charts (Figure 1), and adherence to national guidelines are essential for minimizing risk and protecting patient safety. Continuous monitoring and assessment, using forms like the WHO Hand Hygiene Monitoring Form (Annex 8), are key.
Common Types of HAIs
Several infections frequently manifest as HAIs, posing significant challenges to patient well-being. Catheter-associated urinary tract infections (CAUTIs) are prevalent, alongside central line-associated bloodstream infections (CLABSIs). Surgical site infections (SSIs) represent another common concern, demanding meticulous surgical technique and post-operative care.
Pneumonia, particularly ventilator-associated pneumonia (VAP), also falls within the scope of HAIs. Clostridioides difficile infection (CDI), causing severe diarrhea, is increasingly recognized. Accurate case definitions (Annex 7) are crucial for consistent reporting and surveillance.
Preventive measures tailored to each HAI type are essential, encompassing bundled interventions and adherence to established guidelines. Proactive monitoring and rapid response to potential outbreaks are vital components of a comprehensive infection control strategy.
HAI Reporting and Surveillance
Robust HAI reporting and surveillance systems are fundamental to effective infection control programs. Standardized definitions of HAI cases (Annex 7) ensure consistent data collection and analysis. Accurate reporting allows for trend identification and targeted interventions.
National and local health authorities often mandate HAI reporting, utilizing standardized forms. Surveillance data informs benchmarking, enabling healthcare facilities to compare their performance against peers. Monitoring forms, like the WHO Hand Hygiene Monitoring Form (Annex 8), contribute to broader surveillance efforts.
Data analysis reveals patterns, facilitating the implementation of evidence-based practices to reduce HAI incidence. Continuous surveillance is crucial for early outbreak detection and prompt response.
Specific Infection Control Scenarios
Preparedness is key when facing unique challenges. Protocols for sharps injuries, spill management, and outbreak control are essential for patient safety.
Managing Sharps Injuries

Immediate and proper response to sharps injuries is paramount. Following an accidental needlestick or cut from a sharp object, the incident requires swift action to minimize risk. First, immediately stop the procedure and activate the safety device, if applicable. Then, wash the wound thoroughly with soap and water.
Crucially, report the incident according to facility policy – documentation is vital for tracking and prevention. Exposure prophylaxis, including post-exposure prophylaxis (PEP) for bloodborne pathogens like HIV and Hepatitis B/C, may be necessary, guided by healthcare professionals and current guidelines.
Complete incident reports and follow-up testing are essential components of a comprehensive sharps injury management plan, ensuring both employee safety and patient protection.
Spill Management Protocols
Effective spill management is critical for preventing the spread of infection. Protocols must address various types of spills – blood, body fluids, or potentially infectious materials – with a standardized approach. Initial steps involve ensuring personal safety, donning appropriate PPE (gloves, gown, mask, eye protection), and restricting access to the area.
Absorbent material should be applied to contain the spill, followed by careful cleaning and disinfection using an approved disinfectant. Proper disposal of contaminated materials as regulated medical waste is essential.
Detailed documentation of the spill, including the date, time, location, type of material, and cleanup procedures, is crucial for tracking and quality improvement efforts. Training staff on these protocols is paramount.
Infection Control During Outbreaks
Outbreak management demands heightened infection control measures. Rapid identification and reporting of suspected outbreaks are the first steps, triggering activation of pre-established outbreak protocols. Enhanced surveillance, including active case finding, becomes essential to determine the extent of the outbreak.
Implementing cohorting or isolation of affected individuals, reinforcing hand hygiene, and optimizing environmental cleaning and disinfection are vital. Consideration should be given to restricting visitors and potentially cancelling elective procedures.
Clear communication with healthcare personnel, patients, and public health authorities is paramount. Utilizing national guidelines and checklists aids a coordinated response.

Resources and Guidelines
Accessing reliable resources is crucial. National and WHO guidelines, alongside checklists and monitoring forms, support effective infection prevention and control practices.
National Guidelines on Infection Prevention and Control
Robust national guidelines are foundational for consistent infection control. Documents, such as those originating from Dushanbe in 2023, provide detailed annexes covering crucial aspects. These include control lists for PIIK, features of disinfection technologies, and self-assessment forms for hand hygiene.

Standardized definitions of Healthcare-Associated Infection (HAI) cases and associated reporting forms are also vital components. Furthermore, WHO hand hygiene monitoring forms are frequently incorporated; These guidelines often outline minimum criteria for Infection Prevention and Control (IPC) implementation across different healthcare levels – primary, secondary, and tertiary – and feature organizational charts detailing management structures. Accessing and adhering to these national directives is paramount for safeguarding patient and staff well-being.
WHO Hand Hygiene Resources
The World Health Organization (WHO) provides invaluable resources for bolstering hand hygiene practices. Central to these offerings are dedicated monitoring forms, designed to assess and improve adherence to recommended protocols. These forms, frequently integrated into national guidelines – as seen in the Dushanbe 2023 documentation – facilitate data collection and analysis;
WHO’s resources extend beyond simple forms, encompassing comprehensive guidance on techniques and the importance of hand hygiene in preventing the spread of infection. Utilizing these tools allows healthcare facilities to systematically evaluate their performance, identify areas for improvement, and ultimately, enhance patient safety. Consistent application of WHO recommendations is a cornerstone of effective infection prevention and control.
Checklists and Monitoring Forms for Infection Control
Effective infection control hinges on diligent monitoring and systematic assessment. National guidelines, such as those developed in Dushanbe in 2023, frequently incorporate detailed checklists – specifically, PIIK control lists – to ensure adherence to established protocols. These tools provide a structured approach to evaluating various aspects of infection prevention.
Furthermore, readily available monitoring forms, including those adapted from WHO resources (Annex 8), allow for quantifiable data collection regarding hand hygiene compliance and HAI case definitions. Regular use of these checklists and forms enables healthcare settings to identify deficiencies, track progress, and demonstrate accountability in maintaining a safe environment for both patients and staff.